Cannabis : An Emerging Treatment for Common Symptoms in Older Adults
https://www.medscape.com/viewarticle/945238
Abstract and Introduction
Abstract
Background/Objectives: Use of cannabis is increasing in a variety of populations in the United States; however, few investigations about how and for what reasons cannabis is used in older populations exist.
Design: Anonymous survey.
Setting: Geriatrics clinic.
Participants: A total of 568 adults 65 years and older.
Intervention: Not applicable.
Measurements: Survey assessing characteristics of cannabis use.
Results: Approximately 15% (N = 83) of survey responders reported using cannabis within the past 3 years. Half (53%) reported using cannabis regularly on a daily or weekly basis, and reported using cannabidiol-only products (46%). The majority (78%) used cannabis for medical purposes only, with the most common targeted conditions/symptoms being pain/arthritis (73%), sleep disturbance (29%), anxiety (24%), and depression (17%). Just over three-quarters reported cannabis “somewhat” or “extremely” helpful in managing one of these conditions, with few adverse effects. Just over half obtained cannabis via a dispensary, and lotions (35%), tinctures (35%), and smoking (30%) were the most common administration forms. Most indicated family members (94%) knew about their cannabis use, about half reported their friends knew, and 41% reported their healthcare provider knowing. Sixty-one percent used cannabis for the first time as older adults (aged ≥61 years), and these users overall engaged in less risky use patterns (e.g., more likely to use for medical purposes, less likely to consume via smoking).
Conclusion: Most older adults in the sample initiated cannabis use after the age of 60 years and used it primarily for medical purposes to treat pain, sleep disturbance, anxiety, and/or depression. Cannabis use by older adults is likely to increase due to medical need, favorable legalization, and attitudes.
Introduction
There is unprecedented interest in the United States in the potential health benefits of cannabis. As of 2020, 33 states have enacted recreational or medical cannabis legislation, which mirrors changing perspectives about cannabis use. For example, support for cannabis legalization has increased from 12% of Americans in 1969 to 67% in 2019.[1] With the enactment of the Farm Bill in 2019,[2] hemp-derived cannabidiol (CBD) products, which contain less than 3% of the psychoactive component tetrahydro-cannabinol (THC), have become more available throughout the country, providing greater access to cannabis for patients.
There is also some evidence that cannabis is useful in addressing chronic medical conditions.[3–6] The National Academies of the Sciences, Engineering, and Medicine published an extensive review in 2017 of the health effects of cannabis, finding empirical evidence for cannabis reducing symptoms ranging from pain, spasticity, tremor, nausea, and, to some extent, sleep.[7] For example, in a placebo-controlled trial that evaluated aerosolized cannabis, there was a decline in pain ratings among patients with diabetic peripheral neuropathy,[8] and another study examining Sativex®, an extract of 1:1 THC/CBD ratio, found cannabis to be associated with an improvement in self-reported sleep quality among chronic pain patients.[9] Additionally, studies show cannabis may serve a palliative role in cancer treatment by ameliorating many of the adverse effects of chemotherapy.[10] Although it is clear more research is needed to prove the potential benefits as well as harms of cannabis in general and especially in older adults,[11–15] it is possible cannabis may serve as an effective treatment or palliative aid for addressing difficult to treat conditions, such as pain and insomnia, in older adults.[16,17]
Indeed, epidemiological studies have shown an increase in cannabis use among older adults. A study by Han and Palamar documented an increase in cannabis use from 2.4% in 2015 to 4.2% in 2018 among adults 65 years and older in the United States.[18] There is also evidence for increased use of cannabis in earlier years.[19,20]
Despite the increasing use of cannabis in older adults, few studies have examined the ways in which cannabis is used. Reynolds et al completed a survey among 345 patients in a geriatrics clinic at the University of Colorado in 2016 to 2017 and found 32% of patients used cannabis at least once in their lifetimes, and the common reasons for cannabis use were for pain and sleep disorders.[21] Lum et al conducted a survey among community-dwelling adults aged 60 years and older in Colorado, and found that older adults were likely to report using cannabis for both recreational and medical purposes and generally thought cannabis had a positive impact on their lives.[22] Brown et al studied data in the Florida Medical Marijuana Use Registry and found that over half of those registered were older adults, and the most common reason for cannabis use was for chronic pain.[23] There have been some studies including older adults that examine how cannabis is used in California,[24–26] a state where medical use has been legalized since 1996 and recreational use since 2016. For example, one survey among patients in a San Francisco dispensary found that older adults were less likely to report problematic cannabis consumption practices compared with younger patients.[24] However, most of these studies were sampled from the community or local dispensaries, and to the best of our knowledge, none has examined this in a geriatrics clinic setting.
More research is needed to delineate administration forms (e.g., smoking, tinctures, topicals), the health conditions and/or symptoms cannabis is being used to treat, the cannabinoid composition (e.g., CBD and THC), and potency and potential adverse effects experienced in this population. Additionally, more research is needed to examine this in a clinic population of older adults specifically within California. To address these gaps in the literature, we conducted a survey at a geriatrics clinic at the University of California, San Diego (UCSD), in La Jolla, CA, to obtain a more detailed picture of cannabis use in these patients.
Methods
Survey Development and Timing of Administration
We conducted an anonymous survey of patients seen in a geriatrics clinic at UCSD. The survey we used was based on two other surveys of cannabis use[21,27] and informed by feedback from clinicians and cannabis experts. Between June 19, 2019, and June 24, 2019, we tested the survey with 84 patients to assess clarity of questions and feasibility of data collection procedures. The final version of the survey was administered between June 28 and September 6, 2019. The survey was designed to be completed in less than 10 minutes.
The survey included questions on demographic information, including age (<65, 65–69, 70–74, 75–79, 80–84, 85–89, and ≥89 years), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, and unknown), sex (male or female), marital status (married or long-term partner, widowed, divorced/separated, single, or never married), and highest level of education achieved (high school or less, some/completed college degree, or graduate and/or advanced degree), followed by a question to ascertain if the respondent had ever used cannabis or cannabis products. Those who answered “no” were informed they had completed the survey and those answering “yes” were asked further questions on cannabis use, including: at what ages in their life they used cannabis (10–20, 21–40 years, etc), and the most recent time cannabis was used (within last 6 months, between 6 months and 3 years, and >3 years ago). As recreational cannabis use was legalized 3 years before the administration of our survey, we asked those who reported use within the past 3 years further questions on cannabis use, including: primary cannabinoid most commonly used (CBD or THC), reasons for use (medical, recreational, or both), source of cannabis acquisition (e.g., dispensary, growing own, or delivery service), frequency of use (daily, weekly, monthly, or yearly), method of use (e.g., edibles, smoking, tinctures, or patches), and others who are aware of patient’s use (e.g., spouse, significant other, healthcare provider, family, or friend). The survey also asked respondents if they had ever experienced negative adverse effects related to cannabis use and, if so, were asked to identify them from a list of 11 choices and one open-ended response option. Respondents were asked to indicate what conditions and/or symptoms they used cannabis to treat from a list of 15 conditions and symptoms, including one open-ended response. For each condition/symptom selected, respondents were asked to rate the helpfulness of cannabis for each (extremely, somewhat, minimally, or not at all helpful). Please see Supplementary Material S1 for a copy of the survey.
Data Collection Procedures
In the clinic, each patient was provided the survey by staff when they checked in for a visit. Patients were informed that the survey was anonymous, and that participation was voluntary. Patients completed the survey in the reception area and placed the survey in a locked box before entering an examination room. To determine the percentage of people who completed the survey, patients were asked to return the survey even if they did not complete it. This study was deemed exempt from institutional review board review by the UCSD Institutional Review Board.
Participants
A total of 601 surveys were distributed, of which 568 were completed (95%). Of those who completed surveys, 73% were aged 75 years and older, 57% were female, and 79% were non-Hispanic White. Fifty-three percent were married/in a long-term relationship, and 85% had at minimum some college education.
Data Analysis
Analyses were completed in three stages. First, we focused on those who used cannabis within the past 3 years, and compared the demographic characteristics between those who used cannabis within past 6 months versus those who used cannabis between 3 years and 6 months ago using chi-squared tests (or Fisher exact tests if cell sizes were too low [<4 observations]). Second, we compared these groups for the items on cannabis use, reported adverse effects, and reasons for use. Third, to explore lifetime patterns of cannabis use, we identified cannabis users who reported using cannabis for the first time as older adults (e.g., current cannabis users reporting no cannabis use before the age of 61 years) and compared this group with those who previously used cannabis. For these analyses, we used chi-squared or Fisher exact tests if cell sizes were too low.
Results
Of the 568 patients who completed surveys, 56 (10%) used cannabis within the past 6 months, 27 (5%) used cannabis between 6 months and 3 years ago, 71 (13%) used cannabis greater than 3 years ago, and 414 (73%) were never users of cannabis products. reports the demographic information of cannabis users (herein defined as those using cannabis within the past 3 years). Most (79%) were between the ages of 65 and 84 years, over half (60%) were female, most (92%) were non-Hispanic White, over half were married or had a long-term partner (58%), and 89% reported at least some postsecondary education. No differences in demographic characteristics were observed between those using cannabis within the past 6 months and those using between 6 months and 3 years ().
Table 1. Demographic Characteristics of Cannabis Users
| Characteristic | Total (N = 83) | Use between 6 mo and 3 y ago (N = 27) | Use within previous 6 mo (N = 56) |
|---|---|---|---|
| Age, y | |||
| <65 | 2 (2) | 0 (0) | 2 (4) |
| 65–74 | 31 (37) | 10 (37) | 21 (38) |
| 75–84 | 35 (42) | 11 (41) | 24 (43) |
| ≥85 | 15 (18) | 6 (22) | 9 (16) |
| Sex | |||
| Female | 50 (60) | 19 (70) | 31 (55) |
| Male | 33 (40) | 8 (30) | 25 (45) |
| Race/ethnicity | |||
| Non-Hispanic White | 76 (92) | 25 (93) | 51 (91) |
| Non-Hispanic Black | 1 (1) | 1 (4) | 0 (0) |
| Hispanic | 5 (6) | 1 (4) | 4 (7) |
| Non-Hispanic Asian | 1 (1) | 0 (0) | 1 (2) |
| Relationship status | |||
| Married or long-term partner | 48 (58) | 12 (44) | 36 (64) |
| Widowed | 20 (24) | 9 (33) | 11 (20) |
| Divorced/separated | 12 (14) | 6 (22) | 6 (11) |
| Single, never married | 3 (4) | 0 (0) | 3 (5) |
| Education | |||
| High school or less | 9 (11) | 3 (11) | 6 (11) |
| Some/completed college degree | 35 (43) | 15 (56) | 20 (37) |
| Graduate and/or advanced degree | 37 (46) | 9 (33) | 28 (52) |
Note: Data are given as number (percentage) of each group. Percentages correspond to column totals. There were no statistical differences across groups.
Table 1. Demographic Characteristics of Cannabis Users
| Characteristic | Total (N = 83) | Use between 6 mo and 3 y ago (N = 27) | Use within previous 6 mo (N = 56) |
|---|---|---|---|
| Age, y | |||
| <65 | 2 (2) | 0 (0) | 2 (4) |
| 65–74 | 31 (37) | 10 (37) | 21 (38) |
| 75–84 | 35 (42) | 11 (41) | 24 (43) |
| ≥85 | 15 (18) | 6 (22) | 9 (16) |
| Sex | |||
| Female | 50 (60) | 19 (70) | 31 (55) |
| Male | 33 (40) | 8 (30) | 25 (45) |
| Race/ethnicity | |||
| Non-Hispanic White | 76 (92) | 25 (93) | 51 (91) |
| Non-Hispanic Black | 1 (1) | 1 (4) | 0 (0) |
| Hispanic | 5 (6) | 1 (4) | 4 (7) |
| Non-Hispanic Asian | 1 (1) | 0 (0) | 1 (2) |
| Relationship status | |||
| Married or long-term partner | 48 (58) | 12 (44) | 36 (64) |
| Widowed | 20 (24) | 9 (33) | 11 (20) |
| Divorced/separated | 12 (14) | 6 (22) | 6 (11) |
| Single, never married | 3 (4) | 0 (0) | 3 (5) |
| Education | |||
| High school or less | 9 (11) | 3 (11) | 6 (11) |
| Some/completed college degree | 35 (43) | 15 (56) | 20 (37) |
| Graduate and/or advanced degree | 37 (46) | 9 (33) | 28 (52) |
Note: Data are given as number (percentage) of each group. Percentages correspond to column totals. There were no statistical differences across groups.
describes the cannabis use characteristics of cannabis users within the past 3 years. Of the 83 users, more than half reported daily or weekly cannabis use. Forty-six percent reported using CBD-only products, and a similar percentage reported using products containing THC. Almost 80% reported using cannabis for medical purposes only; six persons (7%) reported using cannabis for recreational purposes only. Half of respondents obtained cannabis from a dispensary, with the next most common source being from a delivery service or another person. Only 14% reported obtaining cannabis from more than one source. Lotions and tinctures were the most common methods of cannabis use, followed by smoking and edibles, with more than 37% reporting using more than one method of administration. Family members were most likely to know about cannabis use, followed by friends and healthcare providers, with 67% reporting more than one group being aware of the respondent’s cannabis use. Those using cannabis within the past 6 months used more frequently as compared to those using between 6 months and 3 years.
Table 2. Cannabis Use Characteristics of Those Who Used Within Past 3 Years
| Characteristic | Total (N = 83) | Use between 6 mo and 3 y (N = 27) | Use within previous 6 mo (N = 56) |
|---|---|---|---|
| Use frequencya | |||
| Daily | 27 (38) | 1 (4) | 26 (54) |
| Weekly | 11 (15) | 5 (21) | 6 (12) |
| Monthly | 12 (17) | 1 (4) | 11 (23) |
| Yearly or less | 22 (31) | 17 (71) | 5 (10) |
| CBD vs THC | |||
| CBD-only products | 37 (46) | 12 (46) | 25 (45) |
| Products containing THC | 33 (41) | 9 (35) | 24 (44) |
| Not sure | 11 (14) | 5 (19) | 6 (11) |
| Use type | |||
| Medical purposes only | 63 (78) | 20 (74) | 43 (80) |
| Recreational purposes only | 6 (7) | 4 (15) | 2 (4) |
| Both | 12 (15) | 3 (11) | 9 (17) |
| Where obtained cannabis productb | |||
| Dispensary | 45 (56) | 18 (67) | 27 (50) |
| Grow own | 3 (4) | 0 (0) | 3 (6) |
| From someone else | 21 (26) | 8 (30) | 13 (25) |
| Delivery service | 20 (25) | 4 (15) | 16 (30) |
| Grocery store | 2 (2) | 1 (4) | 1 (2) |
| Healthcare provider | 1 (1) | 0 (0) | 1 (2) |
| Administration forms usedb | |||
| Smoking | 25 (30) | 12 (44) | 13 (24) |
| Vaping concentrate (e.g., vape pen) | 11 (13) | 4 (15) | 7 (13) |
| Vaping flower | 3 (4) | 0 (0) | 3 (5) |
| Edibles | 21 (26) | 8 (30) | 13 (24) |
| Patches | 1 (1) | 0 (0) | 1 (2) |
| Tinctures | 29 (35) | 11 (41) | 18 (33) |
| Pills | 8 (10) | 3 (11) | 5 (9) |
| Lotion | 29 (35) | 8 (30) | 21 (38) |
| Dabbing | 0 (0) | 0 (0) | 0 (0) |
| Suppository | 0 (0) | 0 (0) | 0 (0) |
| Who knows about useb | |||
| Healthcare provider | 34 (41) | 8 (30) | 26 (47) |
| Family member | 77 (94) | 25 (93) | 52 (95) |
| Friends | 41 (50) | 13 (48) | 28 (51) |
| No one | 3 (4) | 1 (4) | 2 (4) |
| Unsure | 3 (4) | 1 (4) | 2 (4) |
Note: Data are given as number (percentage) of each group. Percentages correspond to column totals. Abbreviations: CBD, cannabidiol; THC, tetrahydrocannabinol.
aStatistically significant at P < .05 from chi-squared or Fisher exact tests.
bIndividuals were asked to check as many response options as applicable for “Where obtained cannabis product,” “Administration forms used,” and “Who knows about use,” and therefore percentages do not add to 100%.
Figure 1 shows the frequency of conditions and/or symptoms for which respondents used cannabis. The most common conditions/symptoms reported were pain/arthritis (73%), sleep disturbance (29%), and anxiety (24%). On average, over three-quarters of patients deemed cannabis “somewhat” or “extremely” helpful in managing any of these conditions. Just under 40% reported using cannabis for more than one symptom/condition. Among the 33 respondents who used cannabis for more than one symptom/condition, the most common combinations were pain/arthritis and sleep conditions (24%), depression and anxiety (9%), and pain/arthritis, sleep, depression, and anxiety (9%).
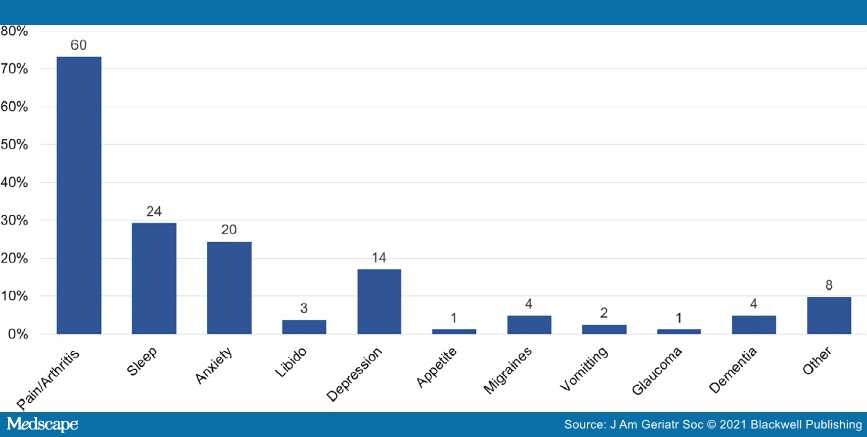 Figure 1.
Figure 1.
Reasons for cannabis use among all users (N = 83). Note: Data label corresponds to N for each reason. Multiple reasons could be chosen. No patients reported use for Parkinson’s disease, epilepsy, multiple sclerosis, and posttraumatic stress disorder. The “other” category includes cancer, high blood pressure, itching, inflammation, and spinal cord injury.
Twelve users (15%) reported experiencing adverse effects, with the most common being dizziness (N = 5), followed by anxiety (N = 3), dry mouth, panic attack, paranoia, unsteadiness, agitation, and other (N = 2 for each), and dry eyes and forgetfulness (N = 1 for each). Among those reporting adverse effects, individuals reported on average 1.83 (standard deviation = 1.19) adverse effects.
Of the 82 respondents who completed questions on ages in which cannabis was used during their lifetime, 61% used cannabis for the first time as adults aged 61 years or older (). Compared with those who used cannabis in the past, those who used cannabis for the first time as older adults were more likely to be older, use CBD-only products, use cannabis for medical purposes, use lotions, and report their healthcare provider being aware of their cannabis use, and were less likely to consume cannabis via smoking or via edibles (P < .05 for all).
Table 3. Cannabis Use Characteristics Comparing Those Who Used Cannabis for the First Time as Older Adults Versus Those Who Used Cannabis Earlier in Life
| Characteristic | Used in past (N = 32) | Used for first time as older adult (N = 50) |
|---|---|---|
| Age, ya | ||
| <65 | 1 (3) | 1 (2) |
| 65–74 | 18 (56) | 12 (24) |
| 75–84 | 10 (31) | 25 (50) |
| ≥85 | 3 (9) | 12 (24) |
| Sex | ||
| Female | 16 (50) | 33 (66) |
| Male | 16 (50) | 17 (34) |
| Race/ethnicity | ||
| Non-Hispanic White | 31 (97) | 44 (88) |
| Non-Hispanic Black | 0 (0) | 1 (2) |
| Hispanic | 1 (3) | 4 (8) |
| Non-Hispanic Asian | 0 (0) | 1 (2) |
| Relationship status | ||
| Married or long-term partner | 21 (66) | 26 (52) |
| Widowed | 5 (16) | 15 (30) |
| Divorced/separated | 3 (9) | 9 (18) |
| Single, never married | 3 (9) | 0 (0) |
| Education | ||
| High school or less | 2 (6) | 7 (14) |
| Some/completed college degree | 15 (47) | 20 (41) |
| Graduate and/or advanced degree | 15 (47) | 22 (45) |
| Use frequency | ||
| Daily | 8 (27) | 18 (44) |
| Weekly | 7 (23) | 4 (10) |
| Monthly | 5 (17) | 7 (17) |
| Yearly or less | 10 (33) | 12 (29) |
| CBD vs THCa | ||
| CBD-only products | 9 (28) | 28 (57) |
| Products containing THC | 17 (53) | 16 (33) |
| Not sure | 6 (19) | 5 (10) |
| Use typea | ||
| Medical purposes only | 16 (52) | 47 (94) |
| Recreational purposes only | 5 (16) | 1 (2) |
| Both | 10 (32) | 2 (4) |
| Where obtained cannabis productb | ||
| Dispensary | 18 (56) | 27 (55) |
| Grow own | 3 (9) | 0 (0) |
| From someone else | 9 (28) | 12 (25) |
| Delivery service | 9 (28) | 11 (22) |
| Grocery store | 1 (3) | 1 (2) |
| Healthcare provider | 0 (0) | 1 (2) |
| Administration forms usedb | ||
| Smokinga | 19 (59) | 5 (10) |
| Vaping concentrate (e.g., vape pen) | 5 (16) | 6 (12) |
| Vaping flower | 3 (9) | 0 (0) |
| Ediblesa | 14 (44) | 7 (14) |
| Patches | 0 (0) | 1 (2) |
| Tinctures | 9 (28) | 20 (41) |
| Pills | 1 (3) | 7 (14) |
| Lotiona | 7 (22) | 22 (45) |
| Dabbing | 0 (0) | 0 (0) |
| Suppository | 0 (0) | 0 (0) |
| Who knows about useb | ||
| Healthcare providera | 7 (22) | 27 (55) |
| Family member | 30 (94) | 46 (94) |
| Friends | 19 (59) | 21 (43) |
| No one | 2 (6) | 1 (2) |
| Unsure | 2 (6) | 1 (2) |
Note: Data are given as number (percentage) of each group. Percentages correspond to column totals. Abbreviations: CBD, cannabidiol; THC, tetrahydrocannabinol.
aStatistically significant at P < .05 from chi-squared or Fisher exact tests.
bIndividuals were asked to check as many response options as applicable for “Where obtained cannabis product,” “Administration forms used,” and “Who knows about use,” and therefore percentages do not add to 100%.
Discussion
With growing interest in the potential health benefits of cannabis and newer legislation favoring legalization across more states, cannabis use is becoming more common in older adult populations. In this study, we described cannabis use characteristics of patients seen in a geriatrics clinic in California, a state that has a long history of legalized medical cannabis and more recent recreational use. Our study showed that older adults use cannabis primarily for medical purposes to treat a variety of common health conditions, including pain, sleep disturbances, and psychiatric conditions.
Our study findings show strikingly similar findings to other geriatrics clinic-based studies in other states and in community-based samples of older adults.[21–23] Treatment for pain was the most common reason for cannabis use, which is similar to the Reynolds[21] and Brown[23] studies showing pain to be a major reason for use in older populations. The Reynolds[21] study also showed sleep problems to be a common reason for use. We also found three-fourths reported cannabis being helpful for addressing health conditions and with few adverse effects, which confirms findings from the study by Lum et al,[22] also showing older adult users to find cannabis useful.
Notably, as hemp-based CBD products become more available across the United States, older adults who may be concerned about the negative psychoactive effects of THC-containing products may be more willing to use cannabis products that contain primarily CBD and to use them in topical formulations. The recent introduction of CBD-only products may explain our finding that new users of cannabis engaged in substantially less risky consumption practices than those who used cannabis in the past (i.e., used cannabis via lotions and tinctures rather than via edibles or smoking).
Given polypharmacy is common in older adults[28] and results showed cannabis was used primarily for medical conditions, there is a need to determine the ways cannabis can interact with the commonly complex combination of medications in this patient group. In the Brown et al study, older adult cannabis patients were coprescribed a number of other medications, including antidepressants, sedatives (e.g., benzodiazepines), and opioids, among others.[23] Higher doses of cannabinoids have the potential to affect the metabolism of various medications,[29] and thus research examining these potential drug-cannabis interactions is warranted.
At the same time, it is possible that cannabis may play a valuable role in deprescribing efforts of potentially inappropriate medications for older adults. One survey with 9,003 respondents showed that, of the 486 respondents who reported ever using cannabis and opioids in the past year, 41% reported a decrease or cessation of opioid use due to cannabis use.[30] Another cross-sectional survey indicated that cannabis is also being used to substitute for anxiolytics/benzodiazepines and antidepressant medications.[31] It is possible that cannabis, when used selectively and with proper supervision, may help decrease polypharmacy in older persons, and be a potentially safer substitute for medicines, including opioids and benzodiazepines, as well as improve quality of life.
Under half of current users reported telling their healthcare providers about their cannabis use. Past research has shown clinicians, for the most part, are supportive of cannabis for medical use, but they have reservations about the limited evidence base, potential safety issues, and product quality and effectiveness.[32,33] A study by Baumbusch et al found older adult cannabis users discussed cannabis with their healthcare providers; however, the main source of information they received was from nonclinical sources (e.g., friends and media).[34] Incorporating scientifically sound information about cannabis in health professionals’ curricula and ongoing professional education forums may help clinicians feel more comfortable discussing cannabis use with their patients. Including questions on cannabis use as part of medication reconciliation during regular ambulatory visits might also facilitate conversations with patients.
Our study has several limitations. First, the sample size of current users was small (N = 83). Despite this, our study provides some novel insights into cannabis use in older adults. Second, given the sensitivity of the topic, it is possible that respondents may have been reluctant to report cannabis use due to stigma. However, we expect stigma was minimal because the survey was anonymous and California has legalized cannabis for both medical and recreational use. Third, our sample was seen in a clinic located in a relatively affluent and highly educated community. Fourth, the survey was provided in English, and thus our survey only included people who understood this language. Fifth, respondents may not be representative of individuals receiving care in other geographic areas or those within different socioeconomic and demographic groups. Finally, these results may not be generalizable to states where recreational or medical cannabis remains illegal.
In conclusion, our study has augmented what is known about cannabis use in older adults by identifying distinct patterns and characteristics of cannabis use among them, with older adult cannabis users using cannabis primarily for medical reasons and to treat specific conditions. These findings are particularly relevant as they provide an updated picture of cannabis use in a clinic-based sample of older adults in California. It will be important to continue monitoring population-based trends in cannabis use in older adults, and identify how the cannabis use characteristics evolve as changes in legalization, availability, formulation, and vehicle of administration occur and evidence of harm and benefit accrues. Further, it is imperative to better understand the efficacy and safety of different formulations of cannabis in treating common conditions in older adults who are heterogeneous in their health and functional status to maximize benefit and minimize harm.
References
- Daniller A. Two-thirds of Americans support marijuana legalization. 2019. https://www.pewresearch.org/fact-tank/2019/11/14/americans-support-marijuana-legalization/. Accessed February 4, 2020.
- Congressional Budget Office. HR 2, Agriculture Improvement Act of 2018, direct spending and revenue effects for the conference agreement on H.R. 2. 2018. http://www.cbo.gov/publication/54880. Accessed September 16, 2020.
- Walsh Z, Callaway R, Belle-Isle L, et al. Cannabis for therapeutic purposes: patient characteristics, access, and reasons for use. Int J Drug Policy. 2013;24(6):511–516.
- Lee G, Grovey B, Furnish T, Wallace M. Medical cannabis for neuropathic pain. Curr Pain Headache Rep. 2018;22(1):8.
- Blake DR, Robson P, Ho M, Jubb RW, McCabe CS. Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology (Oxford). 2006;45(1):50–52.
- Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep. 2017;19(4):23.
- National Academies of Sciences, Engineering, and Medicine. 2017. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: The National Academies Press. https://doi.org/10.17226/24625
- Wallace MS, Marcotte TD, Umlauf A, Gouaux B, Atkinson JH. Efficacy of inhaled cannabis on painful diabetic neuropathy. J Pain. 2015;16(7):616–627.
- Russo EB, Guy GW, Robson PJ. Cannabis, pain, and sleep: lessons from therapeutic clinical trials of Sativex, a cannabis-based medicine. Chem Biodivers. 2007;4(8):1729–1743.
- Abrams DI, Guzman M. Cannabis in cancer care. Clin Pharmacol Ther. 2015;97(6):575–586.
- Grotenhermen F, Müller-Vahl K. Medicinal uses of marijuana and cannabinoids. Crit Rev Plant Sci. 2016;35(5–6):378–405.
- Minerbi A, Hauser W, Fitzcharles MA. Medical cannabis for older patients. Drugs Aging. 2019;36(1):39–51.
- Pratt M, Stevens A, Thuku M, et al. Benefits and harms of medical cannabis: a scoping review of systematic reviews. Syst Rev. 2019;8(1):320.
- van den Elsen GA, Ahmed AI, Lammers M, et al. Efficacy and safety of medical cannabinoids in older subjects: a systematic review. Ageing Res Rev. 2014;14:56–64.
- Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456–2473.
- Ancoli-Israel S, Ayalon L. Diagnosis and treatment of sleep disorders in older adults. Am J Geriatr Psychiatry. 2006;14(2):95–103.
- Larsson C, Hansson EE, Sundquist K, Jakobsson U. Chronic pain in older adults: prevalence, incidence, and risk factors. Scand J Rheumatol. 2017;46(4):317–325.
- Han BH, Palamar JJ. Trends in cannabis use among older adults in the United States, 2015–2018. JAMA Intern Med. 2020;180(4):609–611.
- Lloyd SL, Striley CW. Marijuana use among adults 50 years or older in the 21st century. Gerontol Geriatr Med. 2018;4:2333721418781668.
- Han BH, Palamar JJ. Marijuana use by middle-aged and older adults in the United States, 2015–2016. Drug Alcohol Depend. 2018;191:374–381.
- Reynolds IR, Fixen DR, Parnes BL, et al. Characteristics and patterns of marijuana use in community-dwelling older adults. J Am Geriatr Soc. 2018;66(11):2167–2171.
- Lum HD, Arora K, Croker JA, et al. Patterns of marijuana use and health impact: a survey among older Coloradans. Gerontol Geriatr Med. 2019;5:2333721419843707.
- Brown JD, Costales B, van Boemmel-Wegmann S, Goodin AJ, Segal R, Winterstein AG. Characteristics of older adults who were early adopters of medical cannabis in the Florida medical marijuana use registry. J Clin Med. 2020;9(4):1166.
- Haug NA, Padula CB, Sottile JE, Vandrey R, Heinz AJ, Bonn-Miller MO. Cannabis use patterns and motives: a comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addict Behav. 2017;72:14–20.
- O’Connell TJ, Bou-Matar CB. Long term marijuana users seeking medical cannabis in California (2001–2007): demographics, social characteristics, patterns of cannabis and other drug use of 4117 applicants. Harm Reduct J. 2007;4:16.
- Grella CE, Rodriguez L, Kim T. Patterns of medical marijuana use among individuals sampled from medical marijuana dispensaries in Los Angeles. J Psychoactive Drugs. 2014;46(4):267–275.
- Sexton M, Cuttler C, Finnell JS, Mischley LK. A cross-sectional survey of medical cannabis users: patterns of use and perceived efficacy. Cannabis Cannabinoid Res. 2016;1(1):131–138.
- Qato DM, Wilder J, Schumm LP, Gillet V, Alexander GC. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473–482.
- Qian Y, Gurley BJ, Markowitz JS. The potential for pharmacokinetic interactions between cannabis products and conventional medications. J Clin Psychopharmacol. 2019;39(5):462–471.
- Ishida JH, Wong PO, Cohen BE, Vali M, Steigerwald S, Keyhani S. Substitution of marijuana for opioids in a national survey of US adults. PLoS One. 2019;14(10):e0222577.
- Corroon JM Jr, Mischley LK, Sexton M. Cannabis as a substitute for prescription drugs: a cross-sectional study. J Pain Res. 2017;10:989–998.
- Gardiner KM, Singleton JA, Sheridan J, Kyle GJ, Nissen LM. Health professional beliefs, knowledge, and concerns surrounding medicinal cannabis: a systematic review. PLoS One. 2019;14(5):e0216556.
- Philpot LM, Ebbert JO, Hurt RT. A survey of the attitudes, beliefs and knowledge about medical cannabis among primary care providers. BMC Fam Pract. 2019;20(1):17.
- Baumbusch J, Sloan YI. Exploring new use of cannabis among older adults. Clin Gerontol. 2020;1–7. http://dx.doi.org/10.1080/07317115.2020.1746720.
Previous Presentation
This study was presented at the American Geriatrics Society 2020 Meeting.
Acknowledgments
The authors thank Ian R. Reynolds, MD, Gretchen Orosz, MD, and coauthors for providing access to their survey on cannabis use in older adults.
Financial Disclosure
This work was supported by the National Institute on Aging (T35AG026757, K01AG061239, and P30AG059299), the National Institute on Drug Abuse (K23DA043651), the Stein Institute for Research on Aging, the Center for Healthy Aging, and the Division of Geriatrics and Gerontology at the University of California, San Diego.
Sponsor’s Role
The sponsors of this study had no role in the design, methods, subject recruitment, data collections, analysis, and preparation of article.
J Am Geriatr Soc. 2021;69(1):91-97. © 2021 Blackwell Publishing